CIO #118
Is Apo-B really THAT much more predictive of ASCVD?, Does heavy lifting cause back pain?, Muscle growth tips, and More
Check Out What I’ve Been Checking Out
The Best of What I’m Reading
“Comparison of Conventional Lipoprotein Tests and Apolipoproteins in the Prediction of Cardiovascular Disease”
As I’ve been diving through research on lipidology (i.e. largely triglyceride and cholesterol-related metrics) and cardiovascular disease (CVD), I have shared several papers that suggest that apo-B levels are superior to cholesterol-based metrics (i.e. low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), non-high-density lipoprotein cholesterol (non-HDL-C), etc.) when it comes to risk of CVD.
Interestingly, in their 2019 paper linked above, Welsh and Colleagues came to the contrary conclusion that an apo-B measurement does not add much, if any, predictive value if you already have total cholesterol and HDL-C measurements. (I)
“In conclusion, data from UK Biobank show that the predictive ability of total cholesterol and HDL-C, in the context of other classical risk factors, are not improved by the addition or replacement with apolipoproteins in the assessment of CVD risk. Similarly, non–HDL-C appears adequate to assess on-treatment lipid lowering therapy in this setting. Although lipoprotein(a) measurements may have a role in some settings, these large scale data support the measurement of standard total cholesterol and HDL-C in the nonfasting setting as being perfectly adequate in their capture of lipid-associated CVD risk and for determining non–HDL-C as a treatment target for those already on statins.” (I)
So, how does this fit in with other data on this topic that show apo-B as superior for predicting risk of CVD and atherosclerotic cardiovascular disease in particular?
Well, despite the overarching conclusion quoted above, one piece of the study’s findings does suggest some superiority of apo-B over cholesterol-based metrics: results of the discordance analysis.
As I covered previously in Learning Lipids Part II, discordance in this context describes the scenario where an individual’s apo-B metric does not directionally match their cholesterol-based metrics, namely total cholesterol, LDL-C, or non-HDL-C. In other words their apo-B measurement is high while one or several of those cholesterol-based metric is low, or vice versa.
In Welsh and Colleagues’ paper, they defined this discordance as, “those with an absolute difference of >10 percentage points between their ApoB and [LDL-C] percentiles.” (I)
And, when looking at individuals from their study that fit this definition, they found that LDL-C and non-HDL-C were no longer statistically significantly associated with risk of CVD, while apo-B, HDL-C, and apo-A (a particle-based metric similar to apo-B but for HDL particles) still were. (I)
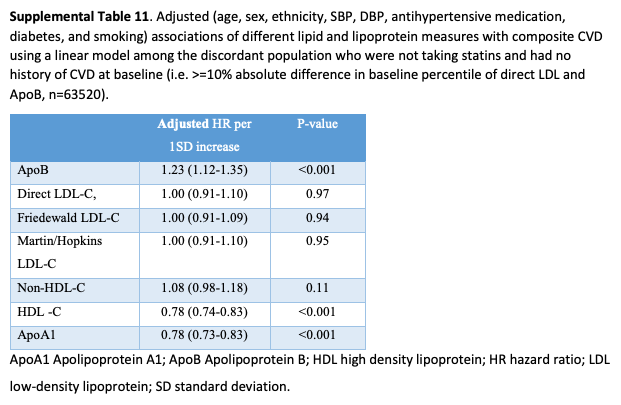
Notably, in this study, ~18% of the subjects met this definition of discordance, which, to me, suggests that–contrary to the study’s overarching conclusion but in line with the other studies I’ve shared that are more bullish on the superiority of apo-B–the apo-B metric is valuable for a significant portion of people. (I)
Still, I think that Welsh and Colleagues’ study offers the takeaway that, despite a lot of emphasis on apo-B, LDL-C and non-HDL-C are generally associated with CVD.



