A couple of months ago, we kicked off the Learning Lipids Series by discussing Cholesterol 101. Now, we’ll continue that conversation and our deep dive into the world of lipidology, as we make sense of the literature regarding lipid metrics and cardiovascular disease (CVD) risk. First, I encourage you to refresh your memory by retrograding to Part I and/or reviewing the highlights I listed below.
Medical Disclaimer: I am not a doctor, and none of the information below is medical advice in any way, shape, or form. Let this post serve as a spark to your curiosity and a stepping stone to conversations with your personal medical providers.
Recap
Cholesterol is a type of lipid, a compound that is nonpolar and does not dissolve in water as a consequence. In order to transport cholesterol and other lipids, your body packages them into protein complexes, called lipoproteins, composed of polar exteriors.
Lipidology can be simplified to the analogy of a highway, where the route represents a blood vessel, the vehicles represent lipoproteins, and the contents carried within/on the vehicles represent lipids.
Metrics Found On a Typical Lipid Panel
High-density Lipoprotein Cholesterol (HDL-C): A measurement of the amount of cholesterol carried by HDL particles in a sample of blood. HDL particles represent one of the 3 major lipoprotein lineages. You can think of the different lineages as analogous to the different types of vehicles on a highway.
Triglycerides (TG): A measurement of the total amount of triglycerides in a sample of blood. Since the majority of triglycerides in your blood are carried by Very Low-density Lipoproteins (VLDLs), this metric is commonly used as a proxy for the amount of VLDL particles in a sample of blood.
Total Cholesterol (TC): A measurement of the total amount of cholesterol in a sample of blood.
Low-density Lipoprotein Cholesterol (LDL-C): A metric of the amount of cholesterol carried by LDL and IDL particles — though the vast majority resides in the LDL particles — in a sample of blood. This metric can be measured directly, or calculated by inputting HDL-C, TC, and TG into Friedewald’s Equation.
Non-HDL-C: A calculation of the amount of cholesterol carried by particles other than HDL particles in a sample of blood.
Particle-based Metrics Not Found On a Typical Lipid Panel
Apolipoprotein-B (Apo-B): A metric of the total amount of particles from the LDL lineage in a sample of blood. This metric leverages the fact that Apo-B 100 proteins are only present on lipoproteins from the LDL lineage — VLDLs, Intermediate-density Lipoproteins (IDLs), Lp(a)s, and LDLs. Since most of the Apo-B-carrying particles in a sample of blood are LDLs, this metric is a proxy for the number of LDL particles in that sample of blood.
LDL-Particle (LDL-P): A metric similar to Apo-B, that measures the total amount of LDL particles in a sample of blood — excluding the VLDL, IDL, and Lp(a) particles that an Apo-B measurement captures. Instead of using Apo-B 100 proteins for measurement, this metric uses nuclear magnetic resonance spectroscopy (NMR) for its measurement.
If my Cholesterol 101 is trash, check out this clip of the renowned Dr. Peter Attia breaking down these concepts for clarity.
Buckle Up
Now that your mind is churning through lipoprotein lineages and interstate analogies – both of which you may be visualizing as The Magic School Bus floating through arteries and veins to the tune of Life Is a Highway by Tom Cochrane – let’s talk about the relevance of the concepts and metrics above.
Since the late 1950s, around when Ancel Keys presented his Diet-Heart Hypothesis based on data from the Seven Countries Study, scientists and physicians have looked to TC as the holy grail of lipid metrics for assessing CVD risk; additionally, as the field has progressed, professionals have incorporated complementary cholesterol-based metrics, such as LDL-C, HDL-C, TG, and Non-HDL-C to better zero in their CVD predictions. In recent years, however, expert cardiologists and lipidologists, like Allan Sniderman and Tom Dayspring, have challenged the status quo of CVD risk assessment, pointing to modern research (I, II) that suggests lipoprotein particle count – specifically the number of particles from the LDL lineage in your blood – is the best predictor of risk, not the mass of lipids carried by those particles. In order to understand this hypothesis, dubbed the Apo-B Particle Model of Atherosclerosis, let’s return to our highway analogy.
Check out this episode from the Attia Drive for a deeper dive on lipids and CVD.
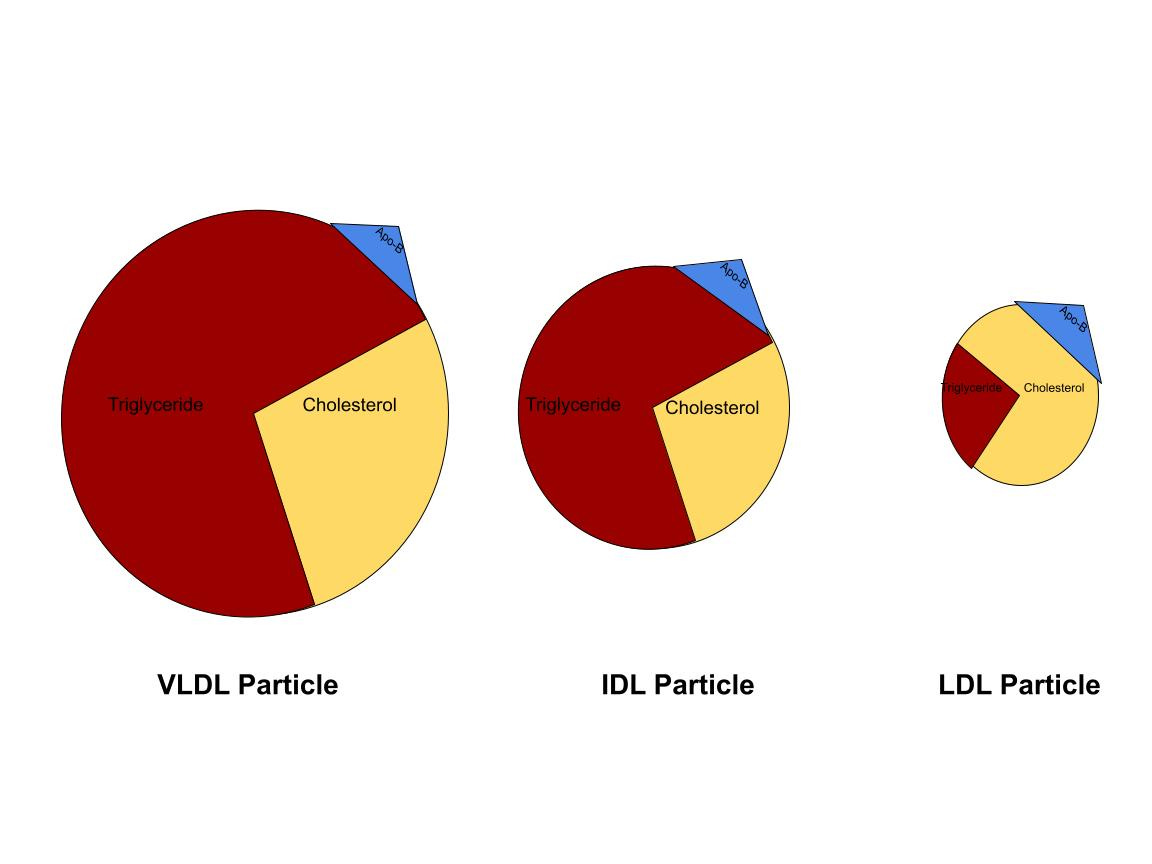
As we covered earlier, you can picture lipoproteins as the vehicles traversing the highway and the different types of vehicles as the different types of lipoproteins – those belonging to the HDL lineage and those belonging to the LDL lineage. For the sake of today’s discussion, forget about HDL particles and solely focus on LDL particles. The LDL lineage is broken down based on density, and each particle’s protein-to-lipid ratio determines its density, in that the greater amount of lipids within the particle, the less dense the particle is and vice versa. Very low-density lipoproteins (VLDLs) sit at the least dense end of the spectrum, as they contain the most amount of triglycerides and cholesterol. As those VLDLs offload lipids to cells throughout the body, they become denser and denser, until they are dense enough to be categorized as intermediate-density lipoproteins (IDLs). The process continues, as the IDLs ultimately relinquish their lipids, increase in density, and become low-density lipoproteins (LDLs). Lipoprotein(a) particles, commonly known as Lp(a) particles, are the last component of the LDL lineage, but, although they are an important piece of the lipidology puzzle, we will leave them aside for the purposes of this post.
When functioning properly, these VLDLs, IDLs, and LDLs make their way through your body – delivering essential lipids to muscle cells and endocrine glands in particular – and return to the liver, where they are removed from circulation and recycled; however, sometimes, these particles find their way into the subendothelial space, or the area between the innermost layer of the blood vessel, the endothelium, and the next layer, the intima. If they become entrapped in this space, these particles can trigger an immune response that ultimately results in plaque formation, known as atherosclerosis. In some ways, this plaque formation, which can lead to rupture and ultimate occlusion of the blood vessel, is similar to the scab development that follows when you scuff your knee on the playground, except it occurs within the blood vessel.
So, for decades, doctors and researchers, following data that correlated LDL-C and TC with increased CVD events, believed that the amount of cholesterol in the blood dictated the probability of the previously described atherosclerotic process occurring. Proponents of the Apo-B Particle Model of Atherosclerosis, on the other hand, believe that the true determinant of atherosclerosis is the concentration of cholesterol-carrying particles, not the quantity of cholesterol itself, in the blood. Imagine that a highway is moderately full of cars carrying a moderate amount of cargo and personnel (Image B below).

Under these circumstances, you guessed it, there would be a moderate risk of an accident taking a car off-road; however, now imagine that, instead of cars, the highway is smothered in motorcycles, each carrying a small amount of cargo (Image C below). Although the total amount of supplies on the highway hasn’t changed, the risk of one of these bikes flying off of the rails and into a tree is – in theory – greater than that of a car from the previous scenario due to the increased congestion.

Similarly, if the highway contained a few 16-wheelers or transit buses transporting large amounts of supplies (Image D below), despite the cargo quantity being unchanged, the risk of catastrophe would – in theory – be decreased due to the relative emptiness of the road.
The Apo-B Particle Model of Atherosclerosis is founded on a similar concept to that underlying these highway scenarios: the risk of a lipoprotein making its way into the subendothelial space depends upon the number of lipoprotein particles traveling in your blood, not by the amount of lipids in your blood.

In defense of this idea, Apo-B supporters offer studies (I, II, III) comparing the risk prediction accuracy of cholesterol-based metrics vs. particle-based metrics when the two are discordant, or do not agree — for example, when LDL-C or Non-HDL-C is high, but Apo-B or LDL-P is low. Whether it be LDL-C or Non-HDL-C compared to LDL-P or Apo-B, when discordance occurs in these studies, the particle-based metrics significantly out-perform the cholesterol-based metrics in terms of risk assessment — meaning that, whether or not the cholesterol-based metrics are high or low, it is the status of the particle-based metrics that correlates with the probability of experiencing a CVD event. Why is this important? Well, if you have high cholesterol, meaning that your LDL-C or Non-HDL-C comes back elevated, but your Apo-B is normal or low, then you could be misled into believing your CVD risk is high when the opposite is the reality. Also, and possibly of more importance, if your cholesterol-based metrics are low, you may be falsely swayed to believe your CVD risk is low; however, if your Apo-B count is high, then your risk of experiencing a CVD event is actually high as well.
Of note, cholesterol-based metrics, such as LDL-C and Non-HDL-C, are often correlated to particle-based metrics, such as Apo-B and LDL-P; yet, research suggests that around 20% of individuals fall into the upper (75th) or lower (25th) quartiles of discordance. For this reason, proponents of the Apo-B Particle Model of Atherosclerosis would suggest that it is essential to acquire an Apo-B count in order to assess a person’s true CVD risk. You may be asking yourself the logical questions, “But why do some people have larger lipoproteins than others, and what determines the concentration of particles in your blood?” For answers and explanations, stay tuned for future parts of the Learning Lipids Series.
References
Glavinovic, T. & Sniderman, A. (2021). Apolipoprotein B: the Rosetta Stone of lipidology. Current Opinion in Endocrinology & Diabetes and Obesity, 28 (2), 90-96. doi: 10.1097/MED.0000000000000596.
Lawler, P. R., Akinkuolie, A. O., Ridker, P. M., Sniderman, A. D., Buring, J. E., Glynn, R. J., Chasman, D. I., & Mora, S. (2017). Discordance between Circulating Atherogenic Cholesterol Mass and Lipoprotein Particle Concentration in Relation to Future Coronary Events in Women. Clinical chemistry, 63(4), 870–879. https://doi.org/10.1373/clinchem.2016.264515
Mora, S., Buring, J. E., & Ridker, P. M. (2014). Discordance of low-density lipoprotein (LDL) cholesterol with alternative LDL-related measures and future coronary events. Circulation, 129(5), 553–561. https://doi.org/10.1161/CIRCULATIONAHA.113.005873
Pischon, T., Girman, C. J., Sacks, F. M., Rifai, N., Stampfer, M. J., & Rimm, E. B. (2005). Non-high-density lipoprotein cholesterol and apolipoprotein B in the prediction of coronary heart disease in men. Circulation, 112(22), 3375–3383. https://doi.org/10.1161/CIRCULATIONAHA.104.532499
Sniderman, A. D., Thanassoulis, G., Glavinovic, T., Navar, A. M., Pencina, M., Catapano, A., & Ference, B. A. (2019). Apolipoprotein B Particles and Cardiovascular Disease: A Narrative Review. JAMA cardiology, 4(12), 1287–1295. https://doi.org/10.1001/jamacardio.2019.3780